All About Lung Biopsies: Procedure, Risks, and What to Expect

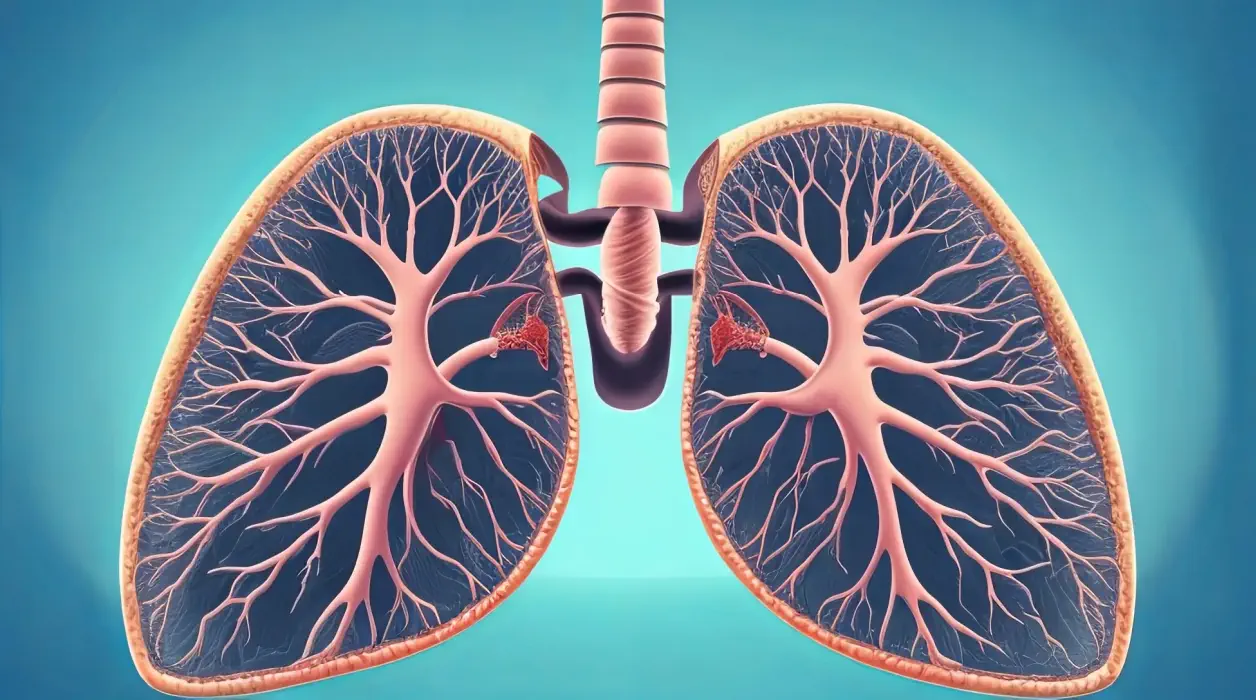
A lung biopsy is a critical medical procedure undertaken to obtain lung tissue for detailed examination under a microscope, often following abnormalities identified in a CT scan or chest X-ray. This process not only facilitates the diagnosis of conditions such as pneumonia, lung cancer, and other pulmonary disorders but also helps in assessing unexplained symptoms like chest pain or shortness of breath. Given its importance, understanding the different methods of lung biopsy, including needle biopsy, transbronchial biopsy through bronchoscopy, and others, is essential for patients and medical professionals alike.
This article will navigate through the intricate details of lung biopsies, from preparation to the biopsy procedure itself, and what patients can expect during recovery. Special attention will be given to the potential risks and complications associated with lung biopsies, such as pneumothorax, to ensure readers are well-informed about all aspects of this diagnostic tool.
Understanding Different Types of Lung Biopsies
Lung biopsies are pivotal in diagnosing and understanding various lung conditions, including lung cancer, pneumonia, and other pulmonary disorders. The choice of biopsy technique depends on the specific condition being investigated, the location of the suspected lesion, and the patient’s overall health status. Below is an overview of the primary lung biopsy procedures, highlighting their methodologies and applications.
- Needle Biopsy:
- Method: Utilizes a hollow needle to remove tissue samples.
- Guidance: Performed under imaging techniques such as CT scan, fluoroscopy, and sometimes ultrasound or MRI to accurately target the lesion.
- Considerations: Less invasive, often not requiring general anesthesia. However, not cost-effective for very small lesions (one to two millimeters in diameter) and may be contraindicated in patients with conditions like emphysema, lung cysts, blood coagulation disorders, insufficient blood oxygenation, pulmonary hypertension, or certain heart failure conditions.
- Surgical Biopsy Techniques:
- Open Biopsy: Involves making an incision in the chest to remove a piece of lung tissue under general anesthesia. It’s typically reserved for cases where larger samples are needed or when other methods are inconclusive.
- Thoracoscopic Biopsy (VATS): A minimally invasive procedure using an endoscope inserted through the chest wall. It allows for the removal of tissue samples with less pain and quicker recovery time compared to open biopsy.
- Percutaneous Transthoracic Lung Biopsy (PTLB) and Open Lung Biopsy (OLB): Both methods involve obtaining tissue samples directly from the lung, with PTLB being less invasive, using CT or fluoroscopic guidance.
- Bronchoscopic Techniques:
- Transbronchial Biopsy (TBLB): Performed through a fiberoptic bronchoscope inserted via the nose or mouth into the lungs, ideal for accessing central lesions.
- Cryobiopsy (Cryo-TBB): Involves freezing and removing tissue using nitrous oxide and a specialized probe, offering a unique approach for certain diagnoses.
- Recent Advances: Techniques such as EBUS (Endobronchial Ultrasound) biopsy, Electromagnetic Navigation Bronchoscopy, Cone Beam CT, and Robotic Bronchoscopy represent the cutting edge in lung biopsy technology, offering enhanced precision and minimized risk.
Each biopsy method has its indications, and contraindications, and requires specific equipment for execution. The choice of procedure is guided by factors such as the suspected condition, lesion size and location, patient health status, and potential risks. Understanding these different types of lung biopsies enables healthcare providers to select the most appropriate method for each patient, optimizing diagnostic accuracy while minimizing complications.
Preparing for a Lung Biopsy
Preparing for a lung biopsy involves several critical steps to ensure the procedure’s safety and effectiveness. Adhering to these guidelines can minimize potential risks and complications:
- Medical Disclosure and Consent:
- Inform your doctor about any recent illnesses, medical conditions, allergies, and medications you’re currently taking.
- It’s essential to disclose if you are pregnant or suspect you might be, as certain types of biopsies may not be recommended.
- You will be required to sign consent papers after the doctor explains the procedure, its risks, and the possibility of more extensive surgery depending on the biopsy results.
- Medication and Dietary Adjustments:
- Medications:
- Stop taking aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs (NSAIDs), as well as blood thinners like warfarin, at least three days before the procedure. Your healthcare provider may provide specific instructions based on your medical history.
- Patients on warfarin or similar anticoagulant medications will need to pause their intake before the test, under the guidance of their healthcare provider.
- Diet:
- Do not eat or drink for 8 hours prior to the biopsy. In some cases, fasting may be required for 6 to 12 hours before the test.
- Medications:
- Physical Preparation:
- Wear loose, comfortable clothing and leave jewelry at home on the day of the procedure.
- You may be asked to change into a hospital gown for the procedure.
- A local anesthetic will be used to numb the area where the biopsy will be taken, ensuring minimal discomfort during the procedure.
Equipment and Safety Measures:
- The procedure room will be equipped with an adult-size flexible bronchoscope with a light source and video monitoring, biopsy forceps, suction apparatus, and an oxygen supply.
- Equipment necessary for cardiopulmonary resuscitation will be readily available in the event of an emergency.
By carefully following these preparation steps, patients can contribute to the success of their lung biopsy procedure and help ensure their safety throughout the process.
The Lung Biopsy Procedure
The lung biopsy procedure varies depending on the type of biopsy being performed, with each method tailored to specific needs and conditions. Below is an overview of the main types of lung biopsies and their procedural specifics:
Needle Biopsy
- Pre-Procedure:
- A chest X-ray or CT scan is conducted to locate the exact spot for the biopsy.
- The patient is seated with arms resting forward on a table.
- The skin at the biopsy site is cleaned, and local anesthesia is administered.
- During the Procedure:
- The doctor makes a small incision in the skin and inserts the biopsy needle into the abnormal tissue or tumor.
- The patient may be asked to hold their breath while the biopsy needle is inserted between the ribs into the lung to obtain a sample.
- The procedure usually lasts 30 to 60 minutes, with the patient given a sedative for relaxation.
- Post-Procedure:
- Firm pressure is applied to the biopsy site until bleeding stops, followed by the application of a bandage.
- A chest X-ray is performed immediately to check for pneumothorax (collapsed lung).
- The tissue sample is sent to a laboratory for analysis, which typically takes a few days.
Transbronchial Biopsy
- During the Procedure:
- Performed under light sedation or local anesthesia.
- The patient may experience discomfort in the throat and have difficulty swallowing for a few days post-procedure.
- Post-Procedure Monitoring:
- Heart rate, oxygen levels, blood pressure, and pain are closely monitored.
- A chest X-ray is taken 3 to 4 hours after the biopsy to ensure no complications have arisen.
Thoracoscopic or Open Lung Biopsy
- Pre-Procedure:
- General anesthesia is used, necessitating fasting for 8 to 12 hours before the biopsy.
- During the Procedure:
- One or more chest tubes may be inserted into the chest cavity to aid in the removal of air or fluid postoperatively.
- Possible complications include blood loss or clots, pain or discomfort, infection, and pneumonia.
- Post-Procedure:
- The patient may need to stay in the hospital overnight for monitoring.
- The lung sample is sent to the lab for examination.
It is important to note that a lung needle biopsy should not be performed if the patient has certain conditions such as a bleeding disorder, bullae, cor pulmonale, cysts of the lung, high blood pressure in the lung arteries, or severe hypoxia. Each procedure entails specific preparation steps, procedural details, and post-procedure care to ensure the safety and effectiveness of the biopsy, with the overarching goal of obtaining accurate diagnostic information while minimizing patient discomfort and potential complications.
Risks and Complications Associated with Lung Biopsies
While lung biopsies are indispensable for diagnosing various lung conditions, they are not without risks and complications. Understanding these potential issues is crucial for patients and healthcare providers to make informed decisions and prepare adequately.
- Common Complications:
- Pneumothorax: Occurs in up to 20.5% of percutaneous chest biopsy cases, with a smaller percentage requiring intervention for chest drainage. This condition involves air leakage into the space between the lung and chest wall, potentially leading to a collapsed lung.
- Pulmonary Hemorrhage: This complication, presenting as coughing up blood, has reported frequencies ranging from 4-27%. It is more likely in patients with small lesion sizes, greater lesion depths, or those with pulmonary arterial hypertension.
- Infection: Any procedure penetrating the skin carries an infection risk. Wound infection, though less common, remains a significant concern following a lung biopsy.
- Rare but Serious Complications:
- Air Embolism: A very rare occurrence with an incidence rate of 0.061% in studies. It can be fatal if air enters the bloodstream, leading to potential heart or brain damage.
- Tumor Seeding: Another rare complication with an incidence rate between 0.012-0.061%, where cancer cells may spread along the needle track, potentially leading to new cancer growths outside the lung.
- Preventive Measures and Management:
- Pneumothorax Management: Includes observation for asymptomatic cases, outpatient management under specific conditions, and confirmation of resolution through follow-up chest radiographs.
- Reducing Pulmonary Hemorrhage Risk: Avoiding biopsy in patients on anticoagulant medication, withholding such medications before the procedure, and careful navigation to avoid major vessels.
- Air Embolism Prevention: Techniques include occluding the introducer needle, advising patients against deep breathing or coughing during the procedure, and avoiding biopsy in certain positions.
Patients are advised to report any symptoms such as shortness of breath, chest pain, difficulty breathing, coughing up blood, fever, chills, or unusual discharge from the biopsy site immediately. Understanding these risks and the measures in place to mitigate them can help manage patient expectations and contribute to the overall safety of lung biopsy procedures.
After the Biopsy: Recovery and Results
After undergoing a lung biopsy, it is imperative for the individual to prioritize rest and adhere to specific post-procedure guidelines to ensure a smooth recovery and the accuracy of the biopsy results. The following points outline key aspects of the post-biopsy phase:
- Recovery Timeline and Activities:
- The recovery period can vary based on the biopsy method used and the individual’s health. It’s crucial to follow the medical professional’s advice on when to resume normal activities.
- Patients are generally advised to avoid intense physical exertion for several days post-biopsy to prevent complications.
- Depending on the procedure type, individuals may be discharged a few hours after the biopsy or may require an overnight hospital stay.
- Post-Procedure Care:
- A chest X-ray is often performed shortly after the biopsy to ensure the lungs are functioning correctly and to check for pneumothorax, a potential complication where air leaks into the space between the lung and chest wall.
- The biopsy site requires proper care to avoid infection. Patients will receive specific instructions on how to care for the wound, including when to remove or change dressings.
- Experiencing chest soreness is common; however, any severe pain, difficulty breathing, fever, or unusual discharge from the biopsy site should be reported to a healthcare provider immediately.
- Results and Follow-up:
- The lung biopsy sample is sent to a laboratory for detailed analysis, with results typically available within one to two weeks.
- These results play a critical role in evaluating abnormalities observed in chest X-rays or CT scans, diagnosing lung infections or diseases, investigating unexplained fluid in the lung, and determining the nature of lung masses.
- A follow-up appointment is usually scheduled to discuss the biopsy results, potential treatment options, and next steps in the patient’s care plan.
It is essential for individuals to closely follow post-biopsy instructions and attend all scheduled follow-up appointments to ensure the best possible outcomes from the lung biopsy procedure.