Creatine for Brain Health and Cognitive Ageing
Creatine is often pigeonholed as a gym supplement, but its relevance to brain health has quietly built an evidence base that deserves mainstream attention. Whereas athletes use creatine for quicker recovery and improved power output, researchers now study its role as a bioenergetic support for neurons and glia. The brain is energetically demanding, and when its phosphate energy buffering system falters—during ageing, stress, or injury—creatine can function as a metabolic reserve. This opening paragraph sets the stage for a deeper look at history, mechanisms, clinical trials, cultural reception, and practical guidance. I will avoid marketing fervor and instead trace the data, ambiguities, and real-world implications for people curious about cognitive ageing, mood, and recovery from neurological insult.
Historical context and the slow pivot to neurobiology
Creatine was first isolated in the early 19th century and later linked to muscle physiology; it entered the public consciousness in the late 20th century as a legal, effective ergogenic aid for strength athletes. For decades the conversation centered on skeletal muscle, dosing strategies for performance, and safety in healthy young adults. Only more recently—primarily since the 1990s and accelerating in the 2010s—have neuroscientists applied creatine’s well-characterized role in energy metabolism to brain health. Magnetic resonance spectroscopy (MRS) enabled direct measurement of brain creatine levels, and clinical interest expanded into areas such as traumatic brain injury (TBI), major depressive disorder, and cognitive decline. The historical arc shows how a supplement born out of sports science migrated into neurology and psychiatry, reflecting broader methodological advances and a growing appreciation for bioenergetics as a determinant of mental function.
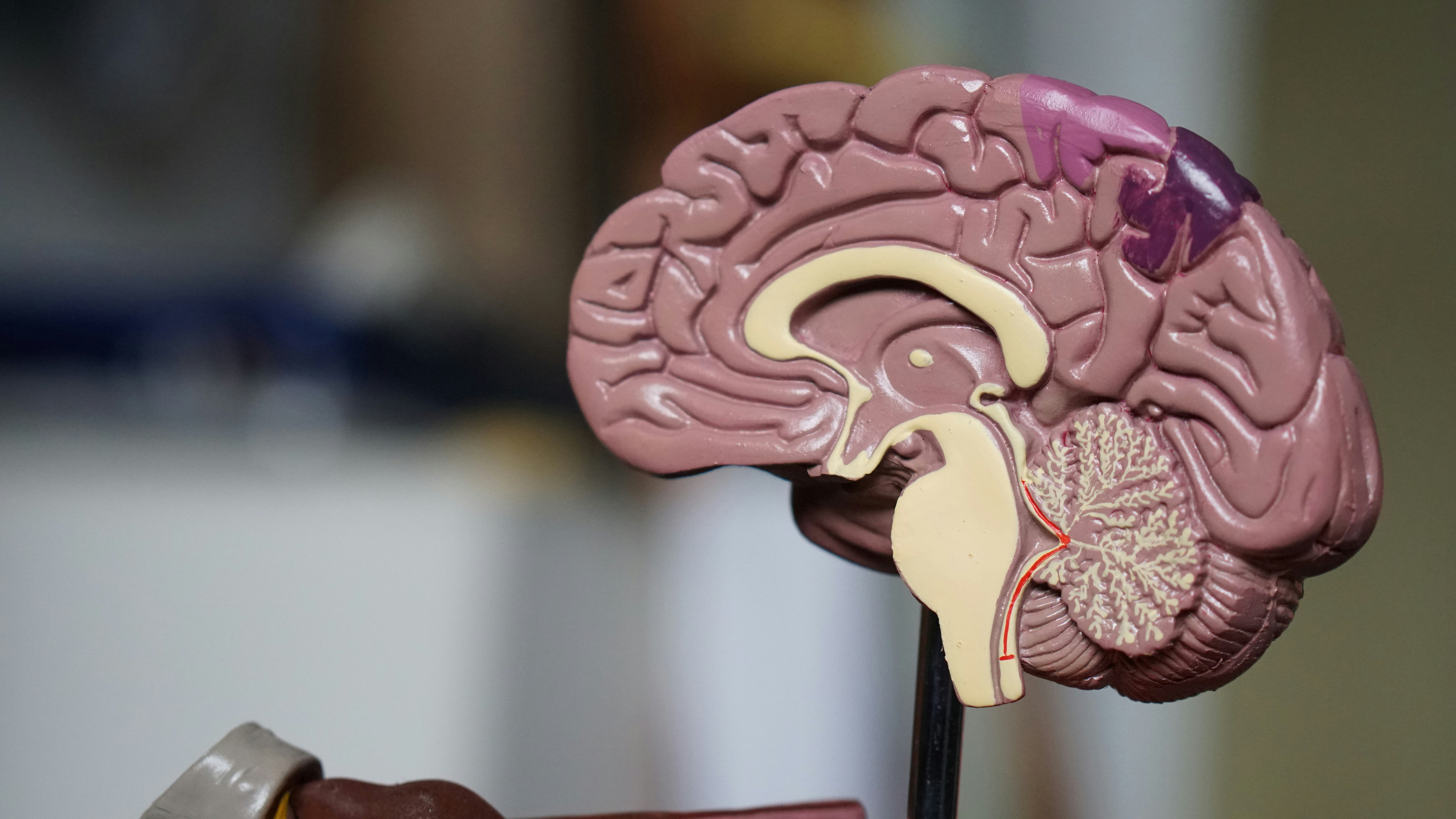
How creatine works in the brain: mechanisms and nuance
At its core, creatine participates in the creatine kinase system: it accepts a phosphate from ATP to form phosphocreatine, which serves as a rapidly mobilizable reservoir to regenerate ATP during high demand. In neurons and astrocytes this buffering is critical for synaptic transmission, ion-pump activity, and maintenance of membrane potentials. Beyond simple phosphate shuttling, creatine influences mitochondrial function, antioxidant defense, and cellular osmoregulation. Important nuances have emerged from basic science: creatine concentrations are not uniform across brain regions, transporter expression (SLC6A8) varies, and certain cell types—like oligodendrocytes—show distinct creatine handling. Genetic defects of the creatine synthesis or transport pathways are rare but informative: they produce severe neurodevelopmental syndromes, proving the molecule’s importance. In ageing or after injury, the local metabolic microenvironment shifts; reduced ATP production and oxidative stress can amplify vulnerability, making an exogenous precursor appealing. However, creatine does not sidestep the complexity of neural networks—its effects are modulatory, and they interact with synaptic plasticity, inflammation, and systemic metabolism.
Clinical evidence: where benefits are clear and where they remain tentative
The clinical literature on creatine and cognition is heterogeneous but increasingly promising in certain niches. In healthy young adults with sufficient dietary intake, cognitive enhancements are modest and often context-dependent—tasks that tax short-term memory under sleep deprivation or mental fatigue show the largest signal. Among vegetarians, who have lower baseline creatine stores due to absence of meat sources, supplementation yields more reliable cognitive gains. In older adults and in mild cognitive impairment, small randomized trials suggest improvements in working memory and executive function, though sample sizes and durations are limited. Creatine has shown potential in acute neurological settings: some trials report reduced biomarkers of neuronal injury and improved outcomes after traumatic brain injury, and preclinical models indicate neuroprotection after ischemic events. Psychiatric applications—particularly for depression and bipolar disorder—are an active area; adjunctive creatine has produced symptomatic improvements in several small trials, possibly through mitochondrial stabilization and modulation of neurotransmitter systems. Notably, outcomes depend on dose, duration, sex, baseline nutrient status, and concurrent therapies. High-quality, large-scale randomized controlled trials are still few, and meta-analyses underscore heterogeneity rather than universal benefit.
Trends, impact, and cultural reception
Public perception of creatine has evolved from a stigmatized “muscle drug” to a mainstream supplement stocked in pharmacies and supermarkets. This trend mirrors broader cultural shifts: a growing appetite for cognitive enhancement, the mainstreaming of nootropics, and increased self-directed health optimization among ageing populations. Social media and wellness influencers have accelerated adoption, often promoting off-label uses and stacking creatine with other supplements like omega-3s, B vitamins, or nicotinamide riboside. Health professionals show mixed responses: some neurologists and psychiatrists recommend short-term trials in specific cases (e.g., treatment-resistant depression, TBI rehabilitation), while others await larger trials. The impact extends to public health conversations about dietary patterns: populations with lower meat consumption may be uniquely positioned to benefit from low-risk supplementation. However, the cultural reception also invites hype—simplistic narratives that suggest creatine is a panacea for cognitive ageing—or unwarranted fears about renal harm. The safety literature, in contrast, supports creatine as well tolerated in recommended doses for most adults, though long-term data in frail elderly populations remain sparse.
Unique insights and research directions not widely covered
Several underreported aspects of creatine biology deserve attention. First, sex differences appear meaningful: women and men may differ in baseline brain creatine, hormonal interactions (estrogen influences on creatine kinase), and clinical response profiles. Few trials stratify by sex, which obscures tailored recommendations. Second, transporter biology matters—SLC6A8 polymorphisms, while rare, may influence uptake efficiency and thus responsiveness to oral creatine; future personalized supplementation could hinge on genotyping. Third, the interaction between creatine and sleep is underexplored. Sleep deprivation increases neural ATP demand and alters creatine metabolism; preliminary studies indicate supplementation can mitigate cognitive losses during acute sleep loss, suggesting situational rather than chronic utility. Fourth, the combination of creatine with cognitive training or physical exercise may be synergistic: exercise enhances mitochondrial biogenesis while creatine buffers acute ATP demand, a pairing that could amplify neuroplasticity, especially in older adults. Finally, the role of creatine in glial-neuronal metabolic coupling—particularly in supporting oligodendrocyte energy needs for myelination—offers a mechanistic link to white-matter integrity in ageing that few clinical studies examine directly.
Practical guidance, safety, and realistic expectations
For clinicians and informed consumers, pragmatic considerations matter. Typical cognitive trials use daily creatine monohydrate doses between 3 and 5 grams after an optional short loading phase; this regimen is inexpensive and accessible. Vegetarians and older adults may show the largest relative gains. Kidney function should be screened in older or medically complex individuals even though creatine is not nephrotoxic in healthy people at standard doses; monitoring creatinine as a renal marker is complicated by creatine’s effect on serum creatinine production and requires clinical context. Side effects are generally mild—weight gain from water retention, gastrointestinal discomfort at high doses, and rare muscle cramping reports. Importantly, creatine is not a substitute for foundational interventions: cognitive stimulation, physical activity, sleep optimization, vascular risk control, and proven pharmacotherapies when indicated. Framing creatine as a potential adjunct—part of a multimodal strategy for brain health—aligns evidence with realistic expectations.
Where policy, practice, and curiosity should go next
The scientific community should prioritize larger, longer trials that stratify by age, sex, diet, and genetic markers of creatine handling, and that measure clinically meaningful endpoints such as functional independence and quality of life. Pragmatic studies embedded in rehabilitation programs (e.g., post-TBI or stroke) could test creatine as a low-cost adjunct to standard care. Regulators and health communicators must also balance accessibility with responsible messaging: avoid turning a modest, evidence-backed tool into a cure-all, while ensuring vulnerable groups who might benefit are not excluded by misinformation. For curious individuals, a short, monitored trial of 3–5 g/day can be reasonable when discussed with a clinician, particularly if other interventions have been exhausted or if diet suggests low baseline stores. Creatine’s journey from locker rooms to laboratories illustrates an important cultural pattern—nutritional molecules can wear many hats—but it also cautions against monocausal explanations for complex brain health challenges.




