Precision Breathwork: Tailoring Breath to Your Physiology
Could breathing be calibrated like an instrument to enhance health and resilience? Recent tools reveal personal respiratory signatures that guide tailored breathing protocols effectively. This article explores historical roots and key scientific breakthroughs in respiratory medicine. You will find evidence, practical testing steps, and personalized protocol examples today. Begin with safe assessments and simple experiments to discover what suits you.

A brief history and scientific foundations
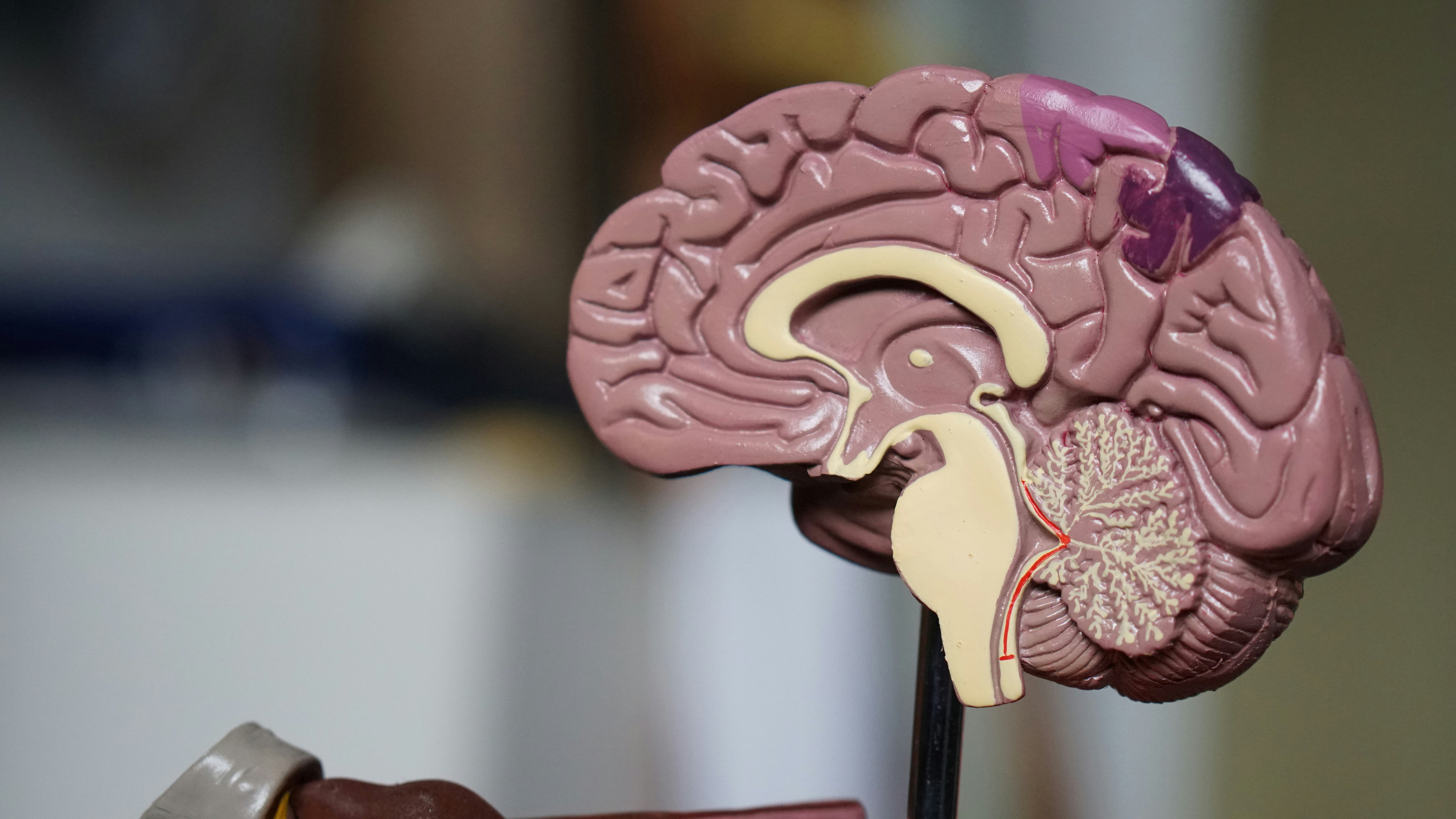
Breath regulation is one of humanity’s oldest self-care practices, from ancient pranayama traditions to indigenous breathing rituals. Modern science began to quantify breathing’s physiological impact in the 19th and 20th centuries with discoveries linking respiration to heart rate variability, baroreflex function, and autonomic control. Key developments included identification of respiratory sinus arrhythmia as a marker of vagal tone and later work mapping how paced breathing at specific frequencies can amplify heart rate variability and baroreflex sensitivity. In recent decades, the integration of capnography, portable heart rate monitors, and neuroimaging has allowed researchers to connect breathing patterns with measurable changes in brain networks involved in emotion regulation, attention, and interoception. These historical and scientific threads set the stage for a new concept: precision breathwork, where individual physiology guides breathing prescriptions rather than one-size-fits-all routines.
Modern respiratory phenotyping: what to measure
Precision breathwork depends on identifying meaningful personal biomarkers. Core measurements include baseline respiratory rate, tidal volume, end-tidal CO2 (a measure of carbon dioxide at the end of exhalation), and heart rate variability metrics such as high-frequency HRV and the amplitude of respiratory sinus arrhythmia. Simple clinical tests such as paced breathing while measuring HRV can reveal a person’s resonance frequency—the breathing rate that maximizes vagal modulation and heart rate oscillation. More advanced phenotyping adds capnography to assess CO2 handling, spirometry for airflow and lung volumes, and symptom questionnaires for dyspnea and hyperventilation tendencies. Wearable sensors now bring many of these measures into everyday settings, enabling longitudinal tracking and dynamic adjustments. The result is a physiological fingerprint that predicts which breathing strategies will likely yield the strongest autonomic and psychological benefits.
Evidence for tailored breathwork: benefits and limitations
A growing body of research supports the therapeutic potential of paced and biofeedback-guided breathing. Randomized controlled trials and meta-analyses indicate that slow, paced breathing can lower blood pressure, improve heart rate variability, and reduce symptoms of anxiety and insomnia. HRV biofeedback—training individuals to breathe at their resonance frequency while viewing real-time HRV—has shown efficacy for anxiety disorders, depression, PTSD, and hypertension in controlled studies. However, responses vary widely between individuals. Some people achieve robust autonomic gains at about six breaths per minute, whereas others respond better to slightly faster or slower rates. CO2 sensitivity also alters outcomes: individuals prone to hypocapnia (low CO2) may experience dizziness and anxiety with certain prolonged exhalation protocols, while those with elevated CO2 tolerance may benefit from breath-hold or cyclical sigh techniques to improve performance and respiratory resilience. Importantly, while many trials show promising effects, heterogeneity in methods and small sample sizes in some studies mean that precision approaches must be implemented with care and ongoing assessment.
Designing personalized breath protocols
Creating a personalized program involves assessment, selection, training, and evaluation. Start with baseline measures: resting respiratory rate, a 5- to 10-minute HRV recording, and a simple CO2 check if feasible (end-tidal measures or standardized breath-hold times as a pragmatic proxy). Perform a resonance frequency test: have the person practice several paced rates between roughly 4.5 and 7 breaths per minute while monitoring HRV amplitude; identify the rate that elicits the largest oscillation. For those with anxiety or panic tendencies, begin with slightly higher rates (for example 7–8 breaths per minute) and prioritize nasal breathing and short practice windows to avoid provoking symptoms. Adjust inhalation-to-exhalation ratios intentionally: longer exhalations tend to promote parasympathetic activity, while balanced or slightly longer inhalations can increase alertness for performance tasks. Incorporate targeted modules such as cyclic sighing for rapid anxiety relief, coherent breathing for daytime regulation, nasal nitric oxide–enhancing breathing for cardiovascular function, and structured breath-hold training for athletes, all tailored to the measured phenotype. Reassess periodically to adapt protocols as physiological markers and subjective outcomes change.
Technology, accessibility, and safety considerations
Advances in wearable HRV monitors, smartphone biofeedback apps, and portable capnography are expanding access to personalized breathwork. Machine learning models can now suggest individualized breathing rates based on large datasets of HRV responses. Yet technology brings caveats: consumer sensors vary in accuracy, and automated recommendations rarely account for medical comorbidities. Safety is paramount. Individuals with uncontrolled hypertension, severe cardiac arrhythmias, epilepsy, pregnancy, or active respiratory infections should consult clinicians before attempting intensive breath training. Those with panic disorder or a history of syncope may require gradual exposure and professional supervision. Practical safeguards include short initial practice durations, slow progression, monitoring for dizziness or chest pain, and terminating exercises if symptoms arise. When implemented responsibly, technology-enhanced precision breathwork can democratize access to individualized respiratory training while maintaining clinical prudence.
Implementation pathways for clinicians and coaches
Clinicians and wellness coaches can integrate precision breathwork by creating assessment workflows and outcome tracking. A practical clinic workflow includes an intake respiratory questionnaire, baseline HRV and respiratory rate measurement, a resonance frequency test, and an initial CO2 tolerance screen. From these data, construct a phased plan: stabilization (gentle paced breathing, nasal focus), adaptation (resonance training or targeted inhalation/exhalation adjustments), and generalization (applying techniques in stressors, sleep onset, or exercise). Use validated outcome measures such as changes in resting blood pressure, HRV indices, validated anxiety or mood scales, and patient-reported functioning. Training professionals in safe cueing techniques and recognition of adverse signs is essential. For performance settings, integrate breathwork with physical warm-ups, mental skills training, and recovery protocols, using objective metrics to demonstrate benefit and refine practice.
Practical breathwork tips and interesting facts
- Begin with five minutes daily of paced breathing at a comfortable rate and gradually increase duration as tolerated.
- Test resonance frequency by trying breathing rates from about five to seven breaths per minute while monitoring heart rate variability; choose the rate that produces the largest, smooth HR oscillations.
- Nasal breathing boosts endogenous nitric oxide production, which supports pulmonary and cardiovascular function; prioritize nasal inhalation when possible.
- If you feel lightheaded during slow breathing, shorten practice sessions and consider increasing CO2 gently by reducing hyperventilatory patterns; consult a professional if symptoms persist.
- Short cyclical sighs (two quick inhales followed by a long slow exhale) can provide rapid anxiety relief and restore calm within 30–60 seconds.
- For athletes, integrating breath-hold sets can improve CO2 tolerance and anaerobic efficiency, but should be done progressively and under guidance.
- Wearables can track HRV trends but may not accurately measure CO2; combine sensor data with subjective reports for better personalization.
- Pregnant individuals and anyone with significant cardiovascular disease should seek clinical clearance before intensive breathwork protocols.
Precision breathwork offers a pragmatic synthesis of ancient practice and modern measurement. By treating respiration as a modifiable physiological parameter and using individualized assessment, people can access targeted strategies that improve autonomic balance, mental regulation, and performance. Start with simple, safe assessments, iterate based on measurements and experience, and seek professional guidance when needed. With thoughtful application, tuning your breath can become a personalized tool for resilience and wellbeing.